We are delighted to share with you the results of the research conducted by Prof. Vivien’s PhIND team (UMR1237, ISERM, UniCaen, Caen), in collaboration with STROK@LLIANCE.
A New Diagnostic Tool for Stroke
Time is Brain. Speed of diagnosis is a critical issue in the treatment of stroke patients. At present, only MRI brain imaging can provide the information needed to make a reliable diagnosis, so that treatment can be tailored to the patient’s situation. In the emergency context, the geographical availability and usage rate of MRIs remains a major obstacle. If we could accelerate diagnosis of hemodynamic abnormalities to distinguish thrombosis from haemorrhage through the use of a convenient and accessible tool, this would represent a significant advance in patient care. It would both improve patient chances of survival and reduce the impact of stroke on long-term functional deficits and quality of life.
The use of functional ultrasound imaging (fUS) opens up precisely such application perspectives. This innovative imaging technique makes it possible to quantify cerebral blood flow with unequalled spatial and temporal resolution, and calculate the volumes of ischemic brain tissue.
This study is the first proof-of-concept of the use of fUS to predict the effectiveness of recanalization in a mouse thromboembolic stroke model. We have achieved this by measuring the impact of a fibrinolytic treatment (rt-PA, Alteplase, BI, Germany) on the evolution of stroke, using two innovative fUS methods (ultrafast ultrasound and ultrasound localization microscopy) in combination with MRI imaging (7T-MRI).
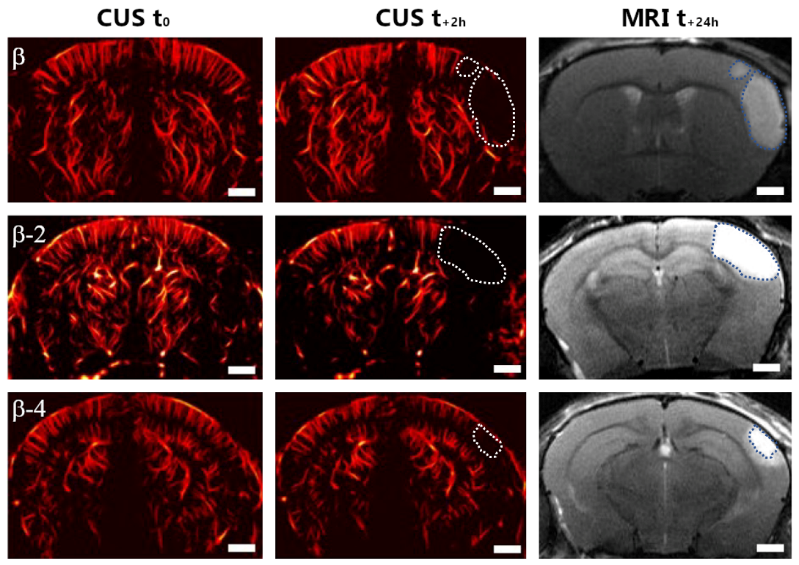
Figure 1: Comparison of ischemic volumes 2 hours post-stroke (CUS t+2h) and 24-hour MRI lesion volumes (MRI t+24h) at different levels of coronal slice versus Bregma (β).
fUS imaging enabled us to monitor ischemia-induced brain hypoperfusion in mice, showing that the ischemic volume measured 2 hours post-stroke does predict the size of the ischemic lesion measured by MRI, 24 hours post-stroke. In addition, partial reperfusion was measured at the same time in mice treated with rt-PA, and also predicts reduced final infarct volume in these mice.
This innovative tool therefore offers high diagnostic value in the clinical management of stroke. It is also of interest for conducting preclinical studies complementary to Doppler technologies (Doppler laser and Doppler speckle) and MRI, both of which provide only semi-quantitative data and are limited in their spatial and temporal resolutions.
We are therefore convinced that ultrafast ultrasound imaging and ultrasound localization microscopy are future-oriented tools for long-term non-invasive monitoring of cerebral blood flow in both clinical and preclinical settings.